A Step-by-Step Guide to Multi-State Licensure for Nurses
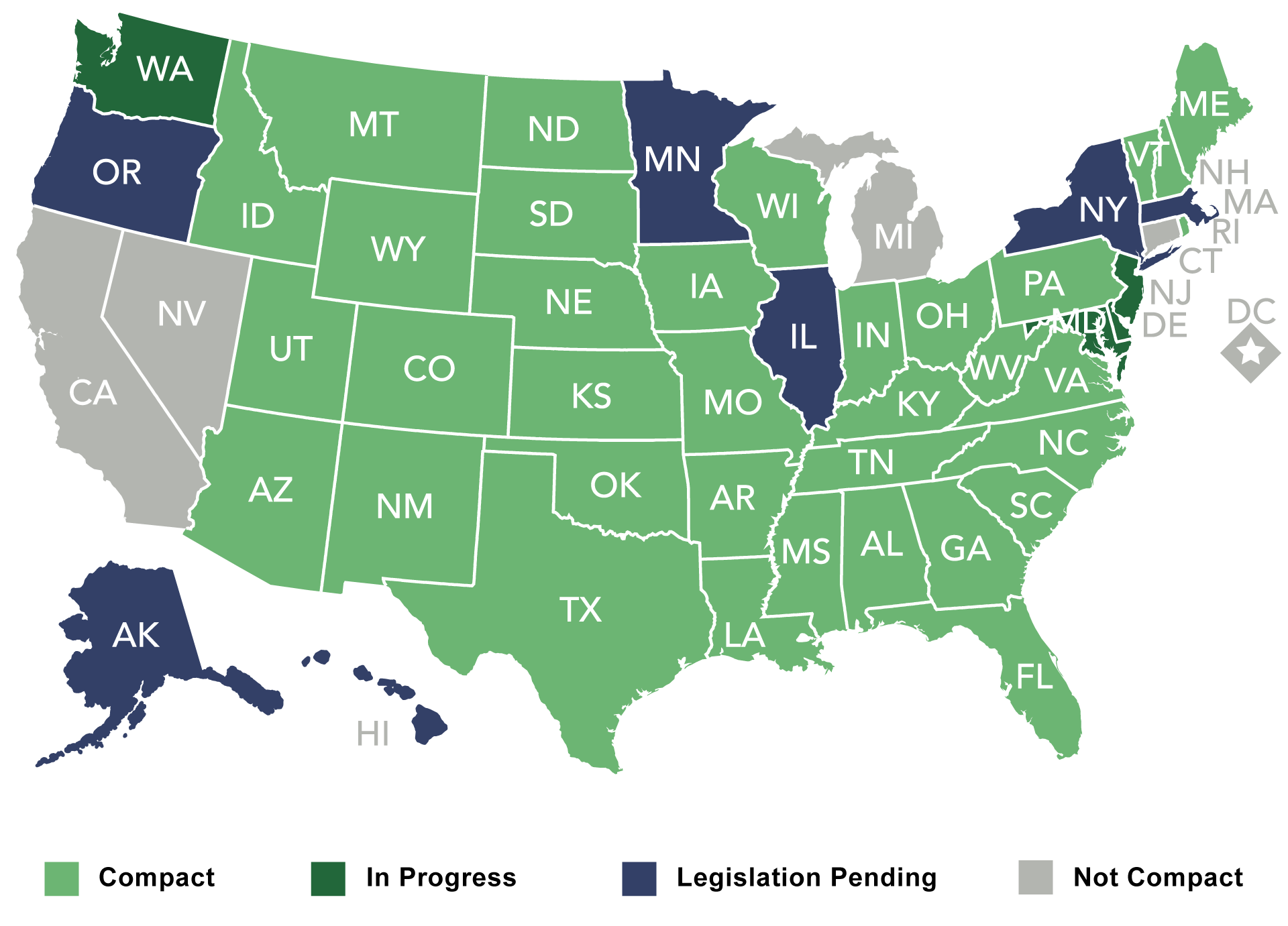
Image Credit: US Nursing
The demands of healthcare worker shortages, soaring numbers of aging adults, and rapid development of telehealth mean that nurses are required to move across regions for extended periods.
The vital importance of a mobile nursing workforce became readily apparent when the COVID-19 pandemic struck. States such as New York and California urgently recruited out-of-state professionals to meet the needs of patients during peak crisis periods.
For nurses, multi-state licensure is not just a career perk that brings unprecedented opportunities. They may be destined for travel nursing assignments in rural areas or telehealth roles helping patients thousands of miles away.
But it can seem daunting to work one’s way through the online tickets before finding a way forward. This guide simplifies the process, providing you with a straight roadmap to securing multi-state licensure through the Nurse Licensure Compact (NLC).
The Nurse Licensure Compact (NLC) Explained
A Brief History of the NLC
Launched in 2000, the NLC was a response to the rising complexity of state-specific licensing laws. By 2018, it had transformed itself into the Enhanced Nurse Licensing Compact (eNLC), which set more demanding requirements for eligibility.
These include federal criminal background checks (and specifications on who may administer them) as well as uniform education standards across all member states. As of 2025, over 40 states have adopted the eNLC, forming a unified multistate licensure system.
How the eNLC Works
Under eNLC, nurses choose a primary state of residence (PSOR). It is the one where they have a driver’s license, vote, and pay taxes. If this state is part of the compact agreement, then the nurse automatically receives a multi-state license.
So even if you have only ever lived in your home state or temporarily reside elsewhere (e.g., during military service), you will still be able to treat patients across the country, you will be able to treat patients all around your country. A nurse residing in Texas (a state in eNLC) is able to treat patients also in Florida or Arizona, without going there to apply for a separate license.
Key Benefits of the eNLC:
- Cost Savings: Avoid paying $200–$400 per state for individual licenses.
- Time Efficiency: Eliminate weeks-long endorsement processes.
- Career Flexibility: Pursue travel nursing, telehealth, or crisis response roles seamlessly.
The Limitations of the eNLC
Not all states participate. Notable holdouts include California, Oregon, and New York, often due to debates over licensing standards or union opposition. Nurses in these states must pursue licensure by endorsement.
Eligibility for Multi-State Licensure
Who Is Eligible for the eNLC?
To practice nursing across state lines, according to the Enhanced Nurse Licensure Compact (eNLC), you must meet four basic criteria. These features consistently emphasize issues like education, ethics, and legal status.
Residency in A Compact State
Your Primary State of Residence (PSOR) must be a member of the eNLC. Residency is not merely a mailing address—it’s a legal designation proven through tangible ties such as a driver’s license, voter registration, or tax filings.
For instance, if you live in Florida but file taxes there and have a Florida driver’s license, then when you leave to work temporarily in Georgia, this still counts as residency back home.
For military families and students who move around a lot, there are exceptions to the residency rule. However, a nurse who leaves the Compact State for non-compact territories — such as California — immediately loses her or his multi-state privileges and has instead to apply individually in every one of these new sites.
Graduate from an Accredited Program
A Nurse Graduate from an Accredited Outside School must choose a school approved by the ACEN or CCNE. This helps guarantee that licensed nurses in any of these compact member states have the same standardized competency.
Nurses trained outside the United States must have their qualifications assessed and certified by bodies like CGFNS International.
Clean Criminal Background
Applicants must pass both state and federal criminal background checks. Some of the common reasons for disqualification usually include felonies, drug-related convictions, or violent misdemeanors.
However, there are details: some states may ignore older convictions or allow appeals on a case-by-case basis. For example, if you had a DUI ten years ago but go through with a state-approved rehabilitation program today, you could still qualify as a Missouri nurse.
Common Pitfalls to Be Avoided
Misunderstandings still prevail while the eNLC brings down barriers to practice in multiple states. A common pitfall is to assume that all compact states apply the same rules.
For example, while Texas renews licenses every two years, Virginia uses a cycle three years long. Ditto with continuing education (CE) requirements: Florida demands classes on medical errors, but Colorado has no CE requirements at all for LPNs.
A nurse relocating from compact-state Arizona to non-compact Oregon. They must apply immediately for an Oregon license because their eNLC privileges terminate once they establish residency somewhere outside of Oregon.
Obtaining a Multi-State License Through the NLC
Step 1: Confirm Your Eligibility
Review your state’s eNLC status from the National Council of State Boards of Nursing (NCSBN) website. Verify your PSOR participation in the eNLC via the National Council Of State Boards Of Nursing Website.
Take New York, for example; it is easy to apply for and receive a multi-state license because it is both a fat state and within the compact states. Nurses in compact states such as North Carolina just apply for a multistate license along with their initial licensure process, for instance.
Nurses from compact states have the simple task of changing a single-state license to the eNLC by providing proof of residency–a process simplified in states like Tennessee, which has online portals for uploading digital copies of driver’s licenses or utility bills.
Step 2: Submit Your Application
Eligible: Review your state’s eNLC status from the National Council of State Boards of Nursing (NCSBN) website. Verify your PSOR participation in the eNLC via the National Council Of State Boards Of Nursing Website.
Take New York, for example; it is easy to apply for and receive a multi-state license because it is both a fat state and within the compact states. Nurses in compact states such as North Carolina just apply for a multistate license along with their initial licensure process, for instance.
Nurses from compact states have the simple task of changing a single-state license to the eNLC by providing proof of residency–a process simplified in states like Tennessee, which has online portals for uploading digital copies of driver’s licenses or utility bills.
Step 3: Navigate the Background Check
FBI and state-level background checks are required in all eNLC states. Nurses from multiple states may expect a delay, as each jurisdiction searches records on its own.
A nurse who lived in New York, Nevada, and then New Mexico probably would spend weeks waiting for each state to affirm their history. Proactive applicants may use third-party services such as IdentoGO to arrange fingerprinting dates well in advance.
Step 4: Await Approval
Processing times vary widely. Texas boasts a swift two-week turnaround, while New Jersey may take three months due to high application volumes.
During this period, nurses can explore job boards like Indeed or specialized platforms like BluePipes to identify opportunities in other compact states.
Licensure by Endorsement in Non-Compact States
However, for nurses practicing in non-eNLC states such as California or Hawaii, multi-state practice involves obtaining individual licensure (typically in each state). It is a cumbersome process, but the good news is that it’s manageable with proper planning.
Step 1: Look Up State Specific Requirements
Each state’s Board of Nursing (BON) has its own set of requirements. California, for example, mandates that RNs complete 30 hours of gerontology continuing education in recognition of the state’s aging population.
New York requires classes in infection control and child abuse reporting; in Hawaii, a notarized “Declaration of Citizenship” form. While the NCSBN has a “Nurse Licensure by Endorsement” tool with checklists, it’s best to contact the BON directly so as not to miss something.
Step 2: Compile Documentation
Most states will request verification of your original license (where it was issued), official transcripts (that have been sealed and sent directly from the university you attended), proof of your recent clinical hours (usually, pay stubs will suffice), and NCLEX scores.
Registered and practical/vocational nurses educated outside the U.S. need to submit credential evaluations from agencies such as CGFNS. The most common delays are transcript requests — Some schools may take weeks to mail documents, so early initiation of requests is essential.
Step 3: Jurisprudence Exam
Some states, such as Texas and Ohio, require nurses to pass an exam on local nursing laws. These tests, often open-book, evaluate knowledge of scope-of-practice rules and ethical guidelines.
Step 4: The temporary permit
One of the loopholes that solve this problem (to an extent) is issuing temporary permits that can be anywhere from 3–6 months (existing in states like Illinois) until the application is reviewed. These permits — priced between 50–50–150 — allow nurses to start work immediately. However , they are non-renewable and become void if the full application is refused.
Special Considerations
The eNLC allows nurses in compact states to provide telehealth care across state lines. What’s more, non-compact states like New York also need separate licenses, even for remote roles.
A telehealth nurse working in Arizona may monitor a patient in Maine but must have a California license to consult with residents of Los Angeles — a complication that should drive careful planning for licensure.
Disciplinary Actions and Multi-State Implications
In 2022, a Tennessee nurse was convicted of DUI and suspended from practice in multiple states, preventing her from practicing in all eNLC states. Because actions in one jurisdiction can have adverse implications in another, legal counsel is vital for responding to BON complaints.
Temporary Licenses for Crisis Response
During disasters such as hurricanes, states like Louisiana offer emergency licenses for 30–90 days. These permits allow for rapid deployment but are not renewable, and nurses must transition to full licensure to take on longer assignments.
Overcoming Challenges
Cost Management
The licensure fee can quickly add up, including application fees ($200 to $400) depending on the state, background checks ($50 to $100), and continuing education (CE) courses that can range anywhere from $20 to $200 a year.
For nurses, especially those who seek to obtain licensure across many states, these costs can be a financial burden.
Although there are travel nursing agencies that can help ease this burden by providing reimbursement for licensing fees, background checks, and continuing education costs. That makes them a powerful option for nurses looking to practice across state lines while minimizing out-of-pocket costs.
Managing Complexity
Expiration alerts are provided through the Nursys e-Notify system, and mentorship and resources are available through professional organizations like the ANA. Nurses who hold more than one license may set aside a “licensure day” each month to keep track of deadlines and requirements.
Relocating to a New State
If you’re changing from a non-compact state to a compact state, you will have to update your PSOR within 30 days. Delays can lead to licensure gaps that put job prospects at risk. Proactive nurses submit residency documents right after relocating.
Ready to start applying across state lines? Check out StaffDNA’s Multistate Job Listings to find the right position for you.
The Future of Nursing Licensure
NLC gaining momentum, with Pennsylvania Vermont eyeing 2024 adoption. Advocates are pushing for a National Nursing License to dissolve state-by-state impediments, but unions resist, fearing diluted advocacy and standards.
In the meantime, technological innovations such as the NCSBN’s real-time licensure dashboard and blockchain credentialing pilots offer the potential to streamline processes, paving the way for a future where nurses practice with historic mobility.